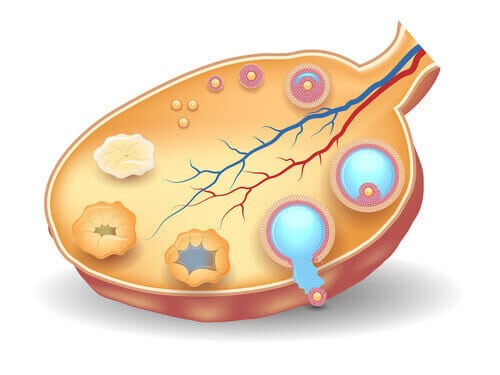
Ovarian reserve is the number of potential oocytes with which a woman is born. It is believed that this is a fixed number for each woman and that throughout life this figure decreases.
By the time a woman reaches puberty, it is believed that she has only 400,000 oocytes of the initial million. With each menstrual cycle, the woman matures a series of follicles so that only one of them matures and can ovulate, making fertilization possible.
The rest of the follicles that were in the maturation process are reabsorbed again and disappear. In each menstruation it is believed that around a thousand oocytes are lost. And with these figures we reach the “critical” age of 35 years, where the ovarian reserve is usually only 10% of the initial figure.
This is the main reason why age is an important determining factor in a woman's fertility. Ovarian reserve determines your fertile period, but it is not always an exact science. To know the fertile capabilities of a woman we must not only look at her ovarian reserve but there are many other factors that influence the scenario.
In fact, it is possible to have a low ovarian reserve and still get pregnant naturally, or to have a high ovarian reserve and encounter difficulties. It is not the most common but it can also happen.
How to measure ovarian reserve
Ovarian reserve can be measured in several ways.
One of them is through a blood test: a quick and fairly simple method, although it is not usually covered by health insurance companies.
In the blood test, the values of the Anti-Müllerian Hormone (AMH). This is a hormone secreted by the sac in which the oocytes mature. For this reason, high levels usually indicate that there are a large number of maturing follicles.
If so, there is a greater chance that one of them will ovulate and pregnancy will be possible. But it is true that there are gynecological conditions such as Polycystic Ovary Syndrome (PCOS) that can offer incorrectly high levels of this hormone.
In PCOS, several of the follicles that were in the process of maturation become encysted within the ovary. This large number of follicles causes a high AMH result.
And yet, it is not a good scenario for fertility.
On the other hand, low levels of this hormone are related to premature ovarian failure, low ovarian reserve or the onset of menopause.
AMH values are generally considered very low if they are below 1.05 ng/ml.
Complementary to this analysis, one should always consider carrying out a ovarian ultrasound looking for antral follicles (small structures in the ovaries where the immature eggs or oocytes are) in the process of development.
The gynecologist can visualize how the woman is responding to the hormonal stimuli of her body. In addition, thanks to ultrasound you can check whether there are growing follicles at the beginning of the cycle or not.
This is a highly validated and used method for assessing ovarian reserve. This method is especially recommended in cases where the AMH has tested low.
Finally, in blood tests it is always interesting to measure the status of the different sex hormones. In particular, the brain hormone that stimulates the ovary for the production and maturation of oocytes.
This hormone is called Follicle stimulating hormone (FSH). If it is very high, it means that the brain is “trying” too hard for its command to be heard by the ovaries. It means that the ovaries are working slower than normal or not working at all.
On the other hand, if FSH is low, we would be in a situation in which the brain itself has decided not to give the order to the ovaries to work. And more research should be done in this regard.
Ovarian reserve: quality better than quantity
We have seen how the level of ovarian reserve is a determining factor when it comes to wanting to get pregnant naturally.
But it is also true when starting fertility treatment through stimulation.
If with the two measurements that we have mentioned (AMH level and ultrasound) it is concluded that there is no base material that can be stimulated, the results of the medication to facilitate the maturation of several oocytes may not have the expected results.
Even so, in cases like this, low stimulation is combined with techniques that favor the quality and development of the material that the woman has. You really only need one viable oocyte. It is always good to bet on quality rather than quantity.
In fact, one of the main fears when stimulating a woman is overstimulation. Too many oocytes usually have abnormalities and are not viable.
It may interest you:
Low Anti-Müllerian Paradox
The human body works like a Swiss watch. It seems to have all the scenarios planned in order to be able to give a fairly efficient response at all times. Avoiding excess and avoiding deficiencies.
This also happens in the area of fertility. The follicle stimulating hormone, FSH, should stimulate, but just enough.
Otherwise, we would run the risk of having multiple pregnancies that would pose a risk to the species. There must be something in the body that puts a brake on FSH, so that it doesn't get out of control.
This is the Anti-Müllerian hormone. That is, given a good response to follicular stimulation, Anti-Müllerian can put a stop to this stimulation. And from here arises the paradox that, when FSH is very low, AMH can also be low, without this implying that there is low ovarian reserve.
Specific fertility treatments for low ovarian reserve
Women with low ovarian reserve are a challenge for fertility treatments. Specific stimulation techniques have been developed for them. And special care is taken to enhance the maturation and development of the few oocytes that can be obtained.
The professional specialist in the matter will give you all the necessary information but do not hesitate to ask about different techniques that are being used today with promising results.
- The use of high doses of gonadotropins.
- The use of low doses of hCG in the first days of ovarian stimulation.
- Double stimulation in the follicular and luteal phase.
- The exacerbation GnRH-a protocol (standard or microdose).
- Stop protocols.
- The luteal onset of Gn RH-a.
- The short protocol.
- The natural cycle or a modified natural cycle seems to be an appropriate strategy.
- Or molecular biology tools (mutations, single nucleotide polymorphisms (SNP)) have also been considered to help the treatment of this group of patients.
Can ovarian reserve be improved?
It could be said that what can be done is not to use up this ovarian reserve faster than normal. For this, there is scientific evidence that supports this option.
There are some factors that worsen ovarian reserve, so avoiding them can help maintain ovarian reserve.
Smoking
Several studies have shown how smoking in women appears to significantly reduce their ovarian reserve and lead to a poor response to ovarian stimulation at an earlier age.
Obesity
In another study, focused on the effects of obesity on fertility, although the antral follicle count did not differ, the Anti-Müllerian hormone did.
The figures of AMH were lower in obese women compared to women of late reproductive age of normal weight.
These data suggest that the lower levels of Anti-Müllerian hormone in obese women of late reproductive age are the result of physiological processes other than the decrease in ovarian reserve itself.
Ovarian surgeries
On the other hand, any type of ovarian surgery usually leads to reductions in the woman's ovarian reserve, with multiple cases of premature ovarian failure. The most common case is the removal of endometriotic ovarian cysts. In any case, more studies are required to clarify whether the damage is related to the surgical procedure or the previous presence of the cysts.
Doubts regarding ovarian reserve and fertility
And finally, there is the question of whether a woman subjected to successive ovarian stimulation could accelerate the loss of her ovarian reserve. Common sense might lead us to think so, but the studies are not conclusive in this regard.
Likewise, it is surprising how women who have been taking contraceptives for several years do not have an ovarian reserve that lasts longer over time. Despite the lack of ovarian activity while taking oral contraceptives, the loss of ovarian reserve seems to respond to other types of stimuli.
Or check how the moment of menarche does not seem to determine the duration of the ovarian reserve either.
It does seem that studies show that there is a genetic bias. Women, daughters of mothers with early menopauses, tend to follow in their mothers' footsteps and have early menopauses.
References:
- Loutradis, D., Drakakis, P., Vomvolaki, E. et al. Different ovarian stimulation protocols for women with diminished ovarian reserve. J Assist Reprod Genet 24, 597–611 (2007). https://doi.org/10.1007/s10815-007-9181-2
- E. Somigliana, G. Ragni, F. Benedetti, R. Borroni, W. Vegetti, PG Crosignani, Does laparoscopic excision of endometriotic ovarian cysts significantly affect ovarian reserve? Insights from IVF cycles, Human Reproduction, Volume 18, Issue 11, November 2003, Pages 2450–2453, https://doi.org/10.1093/humrep/deg432
- Su HI, Sammel MD, Freeman EW, Lin H, DeBlasis T, Gracia CR. Body size affects measures of ovarian reserve in late reproductive age women. Menopause. 2008;15(5):857-861. doi:10.1097/gme.0b013e318165981e
- A El-Nemr, T Al-Shawaf, L Sabatini, C Wilson, AM Lower, JG Grudzinskas, Effect of smoking on ovarian reserve and ovarian stimulation in in-vitro fertilization and embryo transfer., Human Reproduction, Volume 13, Issue 8, Aug 1998, Pages 2192–2198, https://doi.org/10.1093/humrep/13.8.2192
Justin Rashtian & John Zhang (2018) Luteal-phase ovarian stimulation increases the number of mature oocytes in older women with severely diminished ovarian reserve, Systems Biology in Reproductive Medicine, 64:3, 216-219, DOI: 10.1080/19396368.2018.1448902